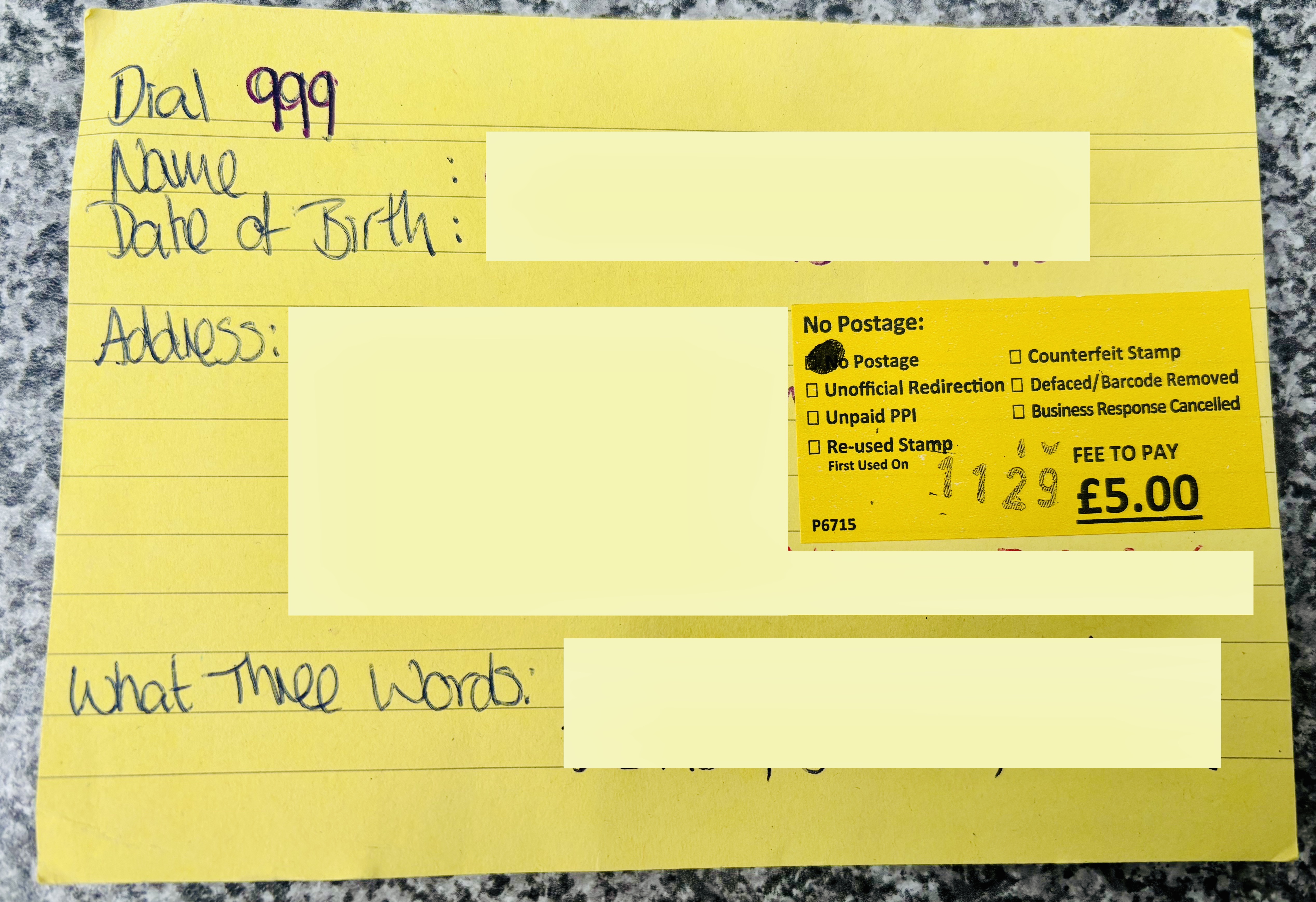
In a post a few weeks ago I mentioned creating ReSPECT forms for Mum and Dad. A few people have asked me about it, and it’s something I was totally unaware of until more recently, so I thought I’d pop a bit of info here.
To make sure I don’t get anything wrong, the following text (apart from my note at the bottom) is lifted direct from The Resuscitation Council UK
What?
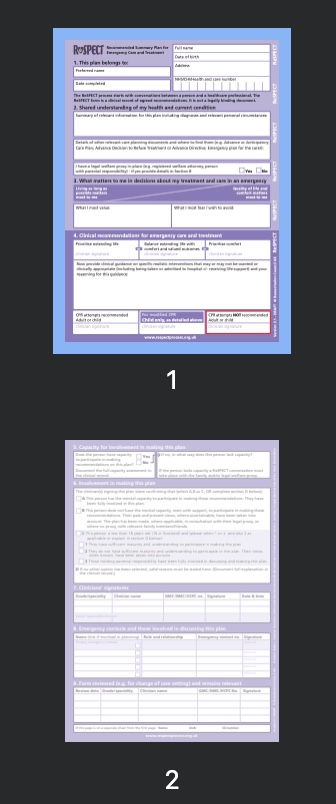
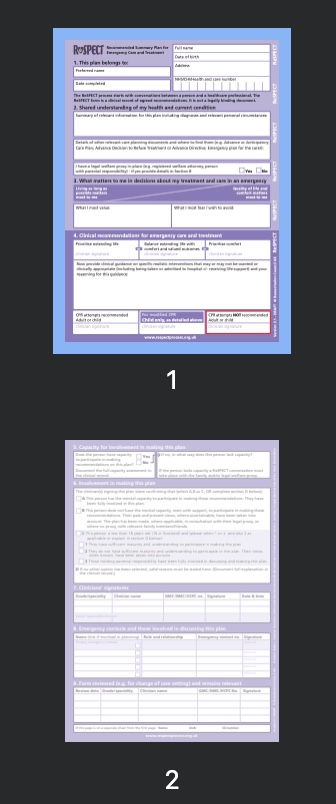
ReSPECT stands for Recommended Summary Plan for Emergency Care and Treatment. The form is not legally binding but they provide valuable guidance that should not be ignored during emergency decision-making.
Why?
The ReSPECT process creates a personalised recommendation for your clinical care in emergency situations, where you are not able to make decisions or express your wishes.
In an emergency, health or care professionals may have to make rapid decisions about your treatment, and you may not be well enough to discuss what is important to you. This plan empowers you to guide them on what treatments you would or would not want to be considered for, and to have recorded those treatments that could be important or those that would not work for you. Many treatments that can be life-sustaining for some people carry a risk of causing harm, discomfort or loss of dignity. Many people choose not to accept that risk if the likelihood of benefit from treatment is small. This plan is to record your preferences and agreed realistic recommendations for emergency situations, whatever stage of life you are at.
ReSPECT may be used across a range of health and care settings, including the person’s own home, an ambulance, a care home, a hospice or a hospital. Professionals such as ambulance crews, out-of-hours doctors, care home staff and hospital staff will be better able to make immediate decisions about a person’s emergency care and treatment if they have prompt access to agreed clinical recommendations on a ReSPECT plan.
Who?
This plan can be for anyone, but will have increasing relevance for people who have complex health needs, people who are likely to be nearing the end of their lives, and people who are at risk of sudden deterioration or cardiac arrest. Some people will want to record their care and treatment preferences for other reasons.
How?
The plan is created through conversations between a person and one or more of the health professionals who are involved with their care. The plan should stay with the person and be available immediately to health and care professionals faced with making immediate decisions in an emergency in which the person themselves has lost capacity to participate in making those decisions.
Where?
This is a UK initiative.
ReSPECT was initially introduced in some localities as part of a formal research evaluation taking place over three years. Alongside this, a network of health and care communities that are adopting and implementing the process is developing. Implementation will be a gradual process, with different health communities adopting and implementing ReSPECT using different timeframes, according to local or regional circumstances. If ReSPECT has already been adopted in your locality then you will be able to work with your health care professional to develop a plan.
Many parts of England and Scotland have now adopted the ReSPECT process, while Northern Ireland and Wales are yet to adopt ReSPECT. Have a read through this data to find out if it’s been adopted where you live.
Note from me:
A DNR or DNACPR (Do not attempt cardiopulmonary resuscitation (CPR)’) form is a separate form specifically about resuscitation in the case of a cardiac arrest or sudden death. (This is not legally binding unless an Advance Decision to Refuse Treatment (ADRT) has been made).
The ReSPECT form states whether a DNR and/or ADRT is in place, but is a much wider document (‘process’ is the correct word according to Google, as it includes the conversations and guidance from a medical professional that are an essential part) covering details including – for example – preference of being treated at home vs hospital and what degree of advanced care the individual feels is appropriate, and where they would prefer to die.
This is rather heavy and made for a few uncomfortable conversations, but to my mind, getting the right care for someone you care about set out (with them where possible) is so important that it’s worth a few moments or ‘urgh’ 😬